Summary on Diagnosis and Natural Treatment of Low Testosterone in Men
What is Low Testosterone?
It is estimated that millions of American men have hypogonadism, which is defined as low serum testosterone with clinical symptoms of androgen deficiency. (1) There is a relative decline in testosterone with increasing chronological age, and there are other health and lifestyle factors that contribute to a decline in this vital hormone. (2,3) The lowering of testosterone is a complex and multifactorial process regulated by the hypothalamic-pituitary-gonadal axis and much controversy exist on the best way to preserve a healthy testosterone level in men. We know from the literature that with male senescence or aging, serum free and total testosterone decline. This leads to increased adiposity which leads to weight gain and obesity which leads to increased circulating estrogen. Since adipose tissue is metabolically active, testosterone gets converted to estradiol via the enzyme aromatase. This excess adipose leads to a vicious cycle of leptin and insulin resistance that leads to the metabolic syndrome with increase in triglycerides (fat in blood) and lower HDL (good cholesterol). Metabolic syndrome is a risk factor for heart disease. (4) There is an association between low testosterone and proven coronary artery disease. (5) Since heart disease is the leading cause of death in America and it is associated with low testosterone, we should take this matter seriously. Physicians should have a high index of suspicion and screen when appropriate and implement a comprehensive strategy to correct this serious problem.
Prevalence
According to the Massachusetts Male Aging Study it is estimated that 2.4 million 40- to 69-yr-old U.S. males have male hypogonadism. Millions more remain undiagnosed. A more recent study examined the prevalence of symptomatic androgen deficiency in men 30 to 79 years of age and found it is 5.6% and increases to 18.4% among 70-year-olds. (6) With aging of the U.S. male population and the current obesity epidemic starting at such a young age which is a risk factor for hypogonadism, the incidence and prevalence of androgen deficiency is likely much higher than estimates from current published studies.
Risk Factors and Cause of hypogonadism
Risk factors for hypogonadism or low testosterone include obesity, metabolic syndrome, type 2 diabetes, over-training syndrome (including marathon training), alcoholism, drug abuse (including chronic marijuana use), chronic stress, osteoporosis, COPD, coronary heart disease, HIV, opiate addiction, inflammatory conditions, cardiac, renal and liver failure, and aging.
The cause of hypogonadism or low testosterone is primary or secondary. In primary hypogonadism the dysfunction originates in the testis and in secondary it originates in the brain.
Primary hypogonadism involves a failure of the testis to produce adequate sperm or testosterone. The causes of primary hypogonadism involve genetic or hereditary causes such as Klinefelter's syndrome, vanishing testes syndrome, Reifenstein’s syndrome, testicular feminization, fertile eunuch syndrome, FSH and LH receptor mutations, cryptorchidism, disorders of androgen biosynthesis, and myotonic dystrophy. Acquired or environmental causes of low testosterone include infections such as mumps orchitis, radiation and chemotherapy, trauma or testicular torsion, systemic diseases, environmental toxins such as xenoestrogen exposure, chronic glucocorticoid, autoimmune damage, and HIV. Many cases of primary hypogonadism are idiopathic (unexplained). (17)
Secondary hypogonadism involves congenital causes or acquired causes. Congenital causes include kallmann’s syndrome, DAX 1 mutation, GPR54 mutation, leptin receptor mutation, Prader Willi, gonadotropin subunit mutation, pituicyte differentiation gene mutations. Acquired causes include hyperprolactinemia, gonadal steroid administration, glucocorticoid treatment, critical illness, chronic systemic illness such as hemochromatosis, chronic opiate use, diabetes mellitus, idiopathic (unexplained), GnRH analogs, benign tumors and cysts, infections, pituitary apoplexy, trauma, surgery, or radiation near the pituitary region. (17)
Diagnosis
The diagnosis is made by a low serum testosterone level in men who are experiencing symptoms of low testosterone. To make the biochemical diagnosis the serum testosterone level should be drawn fasting between 800am and 1000am. A low testosterone level should be confirmed with at least one or two more repeat test. Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) help distinguish between primary and secondary hypogonadism. If the serum testosterone concentration is below normal and the serum LH and FSH concentrations is above normal, then the diagnosis is primary hypogonadism. If the serum testosterone concentration is subnormal and the serum LH and FSH concentrations are normal or reduced, then the diagnosis is secondary hypogonadism. (17)
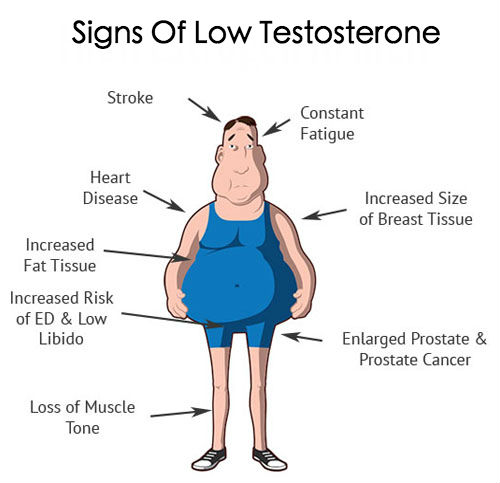
The symptoms of low testosterone are very nonspecific and widespread since testosterone affects many tissues. Symptoms include decreased energy, depressed mood and decreased libido. Those same symptoms could be found in major depressive disorder which can complicate the diagnosis and should be ruled out. Also, decreased muscle mass and reduced physical strength and endurance are nonspecific symptoms associated with many diseases and low testosterone. Decreased body hair loss, and hot flashes may occur, and weight gain is seen in low testosterone and in hypothyroidism, which should be ruled out with a TSH. Some men develop gynecomastia or the enlargement of breast tissue also known colloquially as “man boobs”. Breast cancer and liver disease can cause gynecomastia and those should be ruled out with serum liver function test and a physical exam. Men may also have erectile dysfunction with the loss of morning erections, irritability, loss of motivation and concentration. Again, many of these symptoms are nonspecific and other conditions should be ruled out and excluded and androgen deficiency confirmed with low serum testosterone for age. Based on the clinical picture, a complete workup may include checking levels of prolactin, cortisol, iron, thyroid, MRI of the brain, karyotype, and semen analysis.
Treatment
The first-line therapy for male hypogonadism should be to correct the underlying cause of the problem if possible. For starters, one should control modifiable risk factors such as obesity, sedentary lifestyle, metabolic syndrome, diabetes type 2, chronic stress, poor sleep, alcohol abuse, drug abuse, over-training syndrome and poor dietary habits. Maintain a normal weight and appropriate BMI for one’s body type. This can be done by getting about 1 hour of aerobic exercise on most days of the week as recommended by Institute of Medicine. (18) Also, increased muscle mass and regulating body weight can be achieved by including resistance training of large muscle groups. For example squats, deadlifts, bench press, military press, row machine about 2 or 3 times per week along with aerobic training. Exercise preserves a healthy testosterone level. (7-10) It is important to note that over-training can lead to low testosterone so a proper cycle of rest and recovery should be followed. To ensure adequate recovery from exercise, 8 hours of sleep is recommended. Optimal sleep should be between the hours of 10 p.m. and 600 a.m. Not only is exercise crucial to preserve testosterone levels, but it is necessary for cardiac health. In fact, erectile dysfunction or impotence is often an indicator of atherosclerosis and may precedes a man’s first heart attack by several years.
There is a plethora of literature that shows an association between low endogenous testosterone and coronary artery disease. (16) To address both conditions one should follow a heart-healthy diet that prevents and reverses coronary artery disease. (19-23) Maintaining a healthy heart that allows one to exercise regularly is the foundation to any wellness plan. This is accomplished through a diet that that is organic, whole foods, and plant-based. This dietary approach also helps lower IGF-1 (insulin-like growth factor 1) in men and women. IGF-1 is associated with hormone-dependent cancers such as prostate cancer, breast cancer and colon cancer. (13,14,15) It should be high in vegetables such as kalettes, broccoli, cabbage, and cauliflower. These cruciferous vegetables have indole-3-carbinol which help lower estrogen. These vegetables are also high in fiber which help control weight, regulate blood sugar and lower cholesterol. It should include garlic, which has a compound, diallyl disulfide, that helps increase testosterone and decreases cortisol. (11) Foods high in magnesium such as brazil nuts, seeds, dark leafy veggies, beans, oatmeal, and brown rice are heart healthy and provide the minerals and micronutrients needed for healthy testosterone levels. (12) Adequate zinc in the diet inhibits aromatase and helps preserve healthy testosterone levels. (25) Rich sources of zinc can be found in beans such as chickpeas, mung beans, lentils, cashews, peanut butter, almonds, pumpkin seeds, spinach, cocoa powder, mushrooms, sesame seeds, and quinoa. Also, we know that a low-fat diet can affect our hormonal milieu and the implicated mechanism is a decrease serum cholesterol which decreases serum testosterone. (26-28) However, it is possible to maintain a heart healthy plant-based diet that has 30-40% of calories from fats and keep a high testosterone level. (29) This can be achieved through foods high in monounsaturated and polyunsaturated fats such as avocado, nuts, seeds, olives, and soy, to name a few. One should limit the intake of refined oils and instead eat the natural whole food. An occasional high quality extra virgin olive oil or coconut oil limited to only 1 or 2 tablespoons per day is acceptable. Use caution to ensure the oil is not rancid and limit the intake because it is high calorie and low in micronutrients. Also, recent study shows that coconut oil can increase LDL or bad cholesterol. (30) Another crucial vitamin that also functions as a hormone in the body is vitamin D. For optimal health experts recommend serum levels around fifty international units and a recent study showed that supplementing with vitamin D increased testosterone levels. (25)
Other lifestyle factors that can influence the hypothalamic-pituitary-gonadal axis and decrease testosterone are excessive alcohol intake, chronic stress, and refined sugar. These poor lifestyle habits leads to altered cortisol metabolism, increase adiposity, and lowered testosterone levels. By exercising every day and maintaining a healthy weight, eating a diet that is plant-based and 30 to 40% healthy fats, controlling stress, and getting adequate sleep one can maintain healthy testosterone levels. If hypogonadism is not cured with this all natural lifestyle intervention, then speak to your doctor about a prescription for testosterone and starting TRT (Testosterone Replacement Therapy). TRT leads to substantial improvements in muscle strength and fat-free muscle gain, quality and duration of erections, endurance, improves bone density, improves mood and cognition and overall quality of life in men. There is strong evidence from randomized, controlled trials and experts agree that most men with hypogonadism should be treated unless there is a compelling rationale not to. (Or if patient prefers an all natural approach) In light of emerging literature, I recommend against TRT in men of advanced age, uncontrolled diabetes, uncontrolled hypertension, and a history of heart disease. (31-34) Men on TRT should see their doctor regularly to ensure they are doing well clinically but also to ensure their blood work is within normal parameters.
References
1. Araujo AB, O’Donnell AB, Brambilla DJ, Simpson WB, Longcope C, Matsumoto AM, McKinlay JB. Prevalence and incidence of androgen deficiency in middleaged and older men: estimates from the Massachusetts Male Aging Study. J Clin Endocrinol Metab. 2004;89:5920–5926. 2 J Clin Endocrinol Metab. 2007 Feb;92(2):54955. Epub 2006 Dec 5. The relative contributions of aging, health, and lifestyle factors to serum testosterone decline in men. Travison TG, Araujo AB, Kupelian V, O'Donnell AB, McKinlay JB.
3 J Clin Endocrinol Metab. 2008 Jul;93(7):273745. doi: 10.1210/jc.20071972. Epub 2008 Feb 12. Hypothalamicpituitarytesticular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. Wu FC, Tajar A, Pye SR, Silman AJ, Finn JD, O'Neill TW, Bartfai G, Casanueva F, Forti G, Giwercman A, Huhtaniemi IT, Kula K, Punab M, Boonen S,Vanderschueren D; European Male Aging Study Group. 4 Am J Med. 2006 Oct;119(10):8129. . Metabolic syndrome and risk of cardiovascular disease: a metaanalysis. Galassi A, Reynolds K, He J.Am J Med. 2006 Oct;119(10):8129. 5. Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur Heart J. 2000; 21:890894.
6 J Clin Endocrinol Metab. 2007 Nov;92(11):4241
7. Epub 2007 Aug 14. Prevalence of symptomatic androgen deficiency in men. Araujo AB, Esche GR, Kupelian V, O'Donnell AB, Travison TG, Williams RE, Clark RV, McKinlay JB. 8 Metabolism. 1996 Aug;45(8):9359. Exercise increases serum testosterone and sex hormonebinding globulin levels in older men.Zmuda JM, Thompson PD, Winters SJ.
9 Adaptive Medicine 1(1): 2631, 2009 DOI: 10.4247/AM.2009.AAM004 Exercise and Testosterone TeChi Liu1, ChiaHua Kuo2, and Paulus S. Wang
10 Int J Sports Med. 2004 Nov;25(8):62733. Relationship between diet and serum anabolic hormone responses to heavyresistance exercise in men. Sallinen J, Pakarinen A, Ahtiainen J, Kraemer WJ, Volek JS, Häkkinen K.
11 J Nutr. 2001 Aug;131(8):21506. Garlic supplementation increases testicular testosterone and decreases plasma corticosterone in rats fed a high protein diet. Oi Y, Imafuku M, Shishido C, Kominato Y, Nishimura S, Iwai K.
12 Biol Trace Elem Res. 2011 Apr;140(1):1823. doi: 10.1007/s1201101086763. Epub 2010 Mar 30. Effects of magnesium supplementation on testosterone levels of athletes and sedentary subjects at rest and after exhaustion. Cinar V, Polat Y, Baltaci AK, Mogulkoc R.
13 Cancer Epidemiol Biomarkers Prev. 2002 Nov;11(11):14418. The associations of diet with serum insulinlike growth factor I and its main binding proteins in 292 women meateaters, vegetarians, and vegans. Allen NE, Appleby PN, Davey GK, Kaaks R, Rinaldi S, Key TJ.
14 Cancer Causes Control. 2002 Dec;13(10):92935. Effect of diet and exercise on serum insulin, IGFI, and IGFBP1 levels and growth of LNCaP cells in vitro (United States). Ngo TH, Barnard RJ, Tymchuk CN, Cohen P, Aronson WJ. 15 Am J Clin Nutr. 2005 May;81(5):11637. Association of diet with serum insulinlike growth factor I in middleaged and elderly men. Larsson SC, Wolk K, Brismar K, Wolk A. 16 J Am Heart Assoc. 2013 Nov 15;2(6):e000272. doi: 10.1161/JAHA.113.000272. Testosterone and the cardiovascular system: a comprehensive review of the clinical literature. Oskui PM, French WJ, Herring MJ, Mayeda GS, Burstein S, Kloner RA.
17 Endocr Pract. 2002 NovDec;8(6):44056. American Association of Clinical Endocrinologists Medical Guidelines for clinical practice for the evaluation and treatment of hypogonadism in adult male patients2002 update. Petak SM, Nankin HR, Spark RF, Swerdloff RS, RodriguezRigau LJ; American Association of Clinical Endocrinologists.
18 Panel on Macronutrients, Panel on the Definition of Dietary Fiber, Subcommittee on Upper Reference Levels of Nutrients, Subcommittee on Interpretation and Uses of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes For Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Institute of Medicine; The National Academies Press, Washington, DC, 2005.19 Lancet. 1990 Jul 21;336(8708):12933. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Ornish D , Brown SE , Scherwitz LW , Billings JH , Armstrong WT , Ports TA , McLanahanSM , Kirkeeide RL , Brand RJ , Gould KL .20 JAMA. 1998 Dec 16;280(23):20017. Intensive lifestyle changes for reversal of coronary heart disease.Ornish D , Scherwitz LW , Billings JH , Brown SE , Gould KL , Merritt TA , Sparler S , Armstrong WT , Ports TA ,Kirkeeide RL , Hogeboom C , Brand RJ .21 Am J Cardiol. 2010 Feb 1;105(3):3627. doi: 10.1016/j.amjcard.2009.09.038. Effect of intensive lifestyle changes on endothelial function and on inflammatory markers of atherosclerosis. Dod HS , Bhardwaj R , Sajja V , Weidner G , Hobbs GR , Konat GW , Manivannan S , Gharib W , Warden BE , Nanda NC , Beto RJ , Ornish D ,Jain AC .22 Am J Cardiol. 1999 Aug 1;84(3):33941, A8. Updating a 12year experience with arrest and reversal therapy for coronary heart disease (an overdue requiemfor palliative cardiology). Esselstyn CB Jr .23 J Fam Pract. 1995 Dec;41(6):5608. A strategy to arrest and reverse coronary artery disease: a 5year longitudinal study of a single physician's practice. Esselstyn CB Jr , Ellis SG , Medendorp SV , Crowe TD . 24 Nutrition. 1996 May;12(5):3448. Zinc status and serum testosterone levels of healthy adults. Prasad AS , Mantzoros CS , Beck FW , Hess JW , Brewer GJ . 25 Horm Metab Res. 2011 Mar;43(3):2235. doi: 10.1055/s00301269854. Epub 2010 Dec 10. Effect of vitamin D supplementation on testosterone levels in men. Pilz S , Frisch S , Koertke H , Kuhn J , Dreier J , ObermayerPietsch B , Wehr E , Zittermann A . 26 J Steroid Biochem. 1983 Mar;18(3):36970. Decrease of serum total and free testosterone during a lowfat highfibre diet. Hämäläinen EK , Adlercreutz H , Puska P , Pietinen P . 27 Am J Clin Nutr. 1996 Dec;64(6):8505. Effects of dietary fat and fiber on plasma and urine androgens and estrogens in men: a controlled feeding study. Dorgan JF , Judd JT , Longcope C , Brown C , Schatzkin A , Clevidence BA , Campbell WS , Nair PP , Franz C , Kahle L , Taylor PR . 28 Am J Clin Nutr. 1985 Jul;42(1):12734. Dietary and hormonal interrelationships among vegetarian SeventhDay Adventists and nonvegetarian men. Howie BJ , Shultz TD . 29 Br J Nutr. 1990 Jul;64(1):1119. Testosterone, sex hormonebinding globulin, calculated free testosterone, and oestradiol in male vegans and omnivores. Key TJ , Roe L , Thorogood M , Moore JW , Clark GM , Wang DY . 30. Am J Clin Nutr. 2011 Dec;94(6):14517. doi: 10.3945/ajcn.111.020107. Epub 2011 Oct 26. Diets high in palmitic acid (16:0), lauric and myristic acids (12:0 + 14:0), or oleic acid (18:1) do not alter postprandial or fasting plasma homocysteine and inflammatory markers in healthy Malaysian adults. Voon PT , Ng TK , Lee VK , Nesaretnam K . 31 Increased Risk of NonFatal Myocardial Infarction Following Testosterone Therapy Prescription in Men William D. Finkle1, Sander Greenland2. Gregory K. Ridgeway1 John L. Adams1 Melissa A. Frasco1 Jan201432 Basaria S, Coviello AD, Travison TG, Storer TW, Farwell WR, et al. (2010) Adverse Events Associated with Testosterone Administration. New England Journal of Medicine 363: 109–122. 33 Xu L, Freeman G, Cowling BJ, Schooling CM (2013) Testosterone therapy and cardiovascular events among men: a systematic review and metaanalysis of placebocontrolled randomized trials. BMC Med 11: 108.34 Vigen R, O’Donnell CI, Baro´n AE, Grunwald GK, Maddox TM, et al. (2013) ASsociation of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA 310: 1829–1836. 2013
Comments
Post a Comment